Scientific Insights to Avoid COVID-19
It is fairly easy to avoid getting COVID-19. For most economically secure persons, the risk of COVID is essentially a lifestyle choice; you would balance safety against convenience. The U.S. National Science Foundation (NSF) has funded the VIPRA project for several years on steps to reduce viral infection risk in crowded locations without disrupting human activities. Leveraging our and others’ research, we provide below some science-based insights to help you choose a balance between COVID risk and your desired activities.
Caveat: These tips are based on recent scientific studies and would evolve as scientific knowledge grows. Please talk to your public health official for suggestions based on current local trends. Please note, however, that some of the preventive steps, especially dealing with aerosols, rely on engineering research rather than medical research. There is often a long time lag for such research results to be adopted by public health agencies.
Summary
- A simplified version of this web page is available for those who lack time.
- Young and healthy persons are also now at risk. Even if you get a mild case, “long COVID” can cause long-term problems.
- Social distancing is the most effective technique. But CDC’s recommendation of 6 feet distance is grossly inadequate and simplistic indoors because they did not adequately account for aerosol spread.
- N95 masks can almost eliminate risk in most situations. This can be your key to resuming your normal activities.
- Good ventilation is essential indoors. Keep windows open to the outside and use a portable air purifier with a HEPA filter when the situation warrants.
- You may resume much of your normal activities. You would just need to change how you go about these activities and how often you perform them.
- We focus on preventing COVID. If you are already dealing with COVID, then please look up the list of other resources.

Maintain social distance.
Wear a good mask.

Ventilate your spaces.
Why should you care about COVID risk?
“Isn’t the risk of COVID low for young or healthy persons?” “Don’t most people get only mild symptoms?” You may question whether COVID matters to you. These are legitimate questions.
It is risky to evaluate COVID risk from either the trends with previous strains or the fraction of severe cases. For one, newer strains appear to be affecting more young people than previous ones did. Even the earlier strains affected a larger fraction of young people in India than in the West [Laxminarayan]. In addition, you may experience long-term health repercussions from even mild cases. The so-called “long COVID” leads to various long-term problems, such as those below [CDC-1]. There is also some preliminary evidence that the virus RNA can integrate into the human genome [Zhang].
Long-term effects of COVID include the following [CDC-1].
- Difficulty thinking or concentrating
- Depression and anxiety
- Headache
- Heart palpitations
- Chest pain
- Continued tiredness
- Persistent respiratory tract problems
COVID affects several parts of the body, such as those listed below, and so it is very desirable to avoid the infection [CDC-1].
- Brain
- Kidney
- Heart
- Lung
- Skin
How does COVID spread?
Public health agencies have educated the population of the different mechanisms through which COVID spreads and actions that people can take to avoid COVID. However, not all of these are equally effective. In addition, there are risk factors in developing countries that may not arise in developed ones. It is helpful to understand the different mechanisms and their relative importance so that you can take suitable actions rather than relying on simplistic formulas.
- Droplets: Viruses are embedded in fluid droplets that an infected person may shed while breathing, speaking, or coughing. If you breathe these in, then you could get infected. There may also be some infection risk through your eyes, albeit to a much lower extent. Droplets usually do not travel far, and thus the World Health Organization (WHO) and U.S. Centers for Disease Control and Prevention (CDC) recommend a distance of 3 feet to 6 feet from others to ensure safety. Note that maintaining this distance does not guarantee safety. It is based on old research results. New results show that they can certainly travel around 20 feet [Dbouk], depending on the airflow pattern, and sometimes farther.
- Aerosols: These are like droplets, albeit smaller in size. They can spread much farther than droplets and remain in the air for a long time [Bazant], even after an infective person has left the venue. This is another reason that the 3 feet to 6 feet distancing guideline is inadequate, especially indoors. Good ventilation systems can remove these, and they also dissipate quickly outdoors.
- Fomite: These are viruses that have been deposited on solid surfaces. If you touch such a surface and then put your fingers in your mouth, eyes, or nose, then you could get infected. Disinfection of surfaces has been recommended to avoid this mode of infection spread. But fomite transmission is very rare in developed countries [CDC-2], so this may be a lower priority. On the other hand, such transmission has taken place, and it may play a more significant role in unhygienic surroundings. So, good hygiene is desirable.
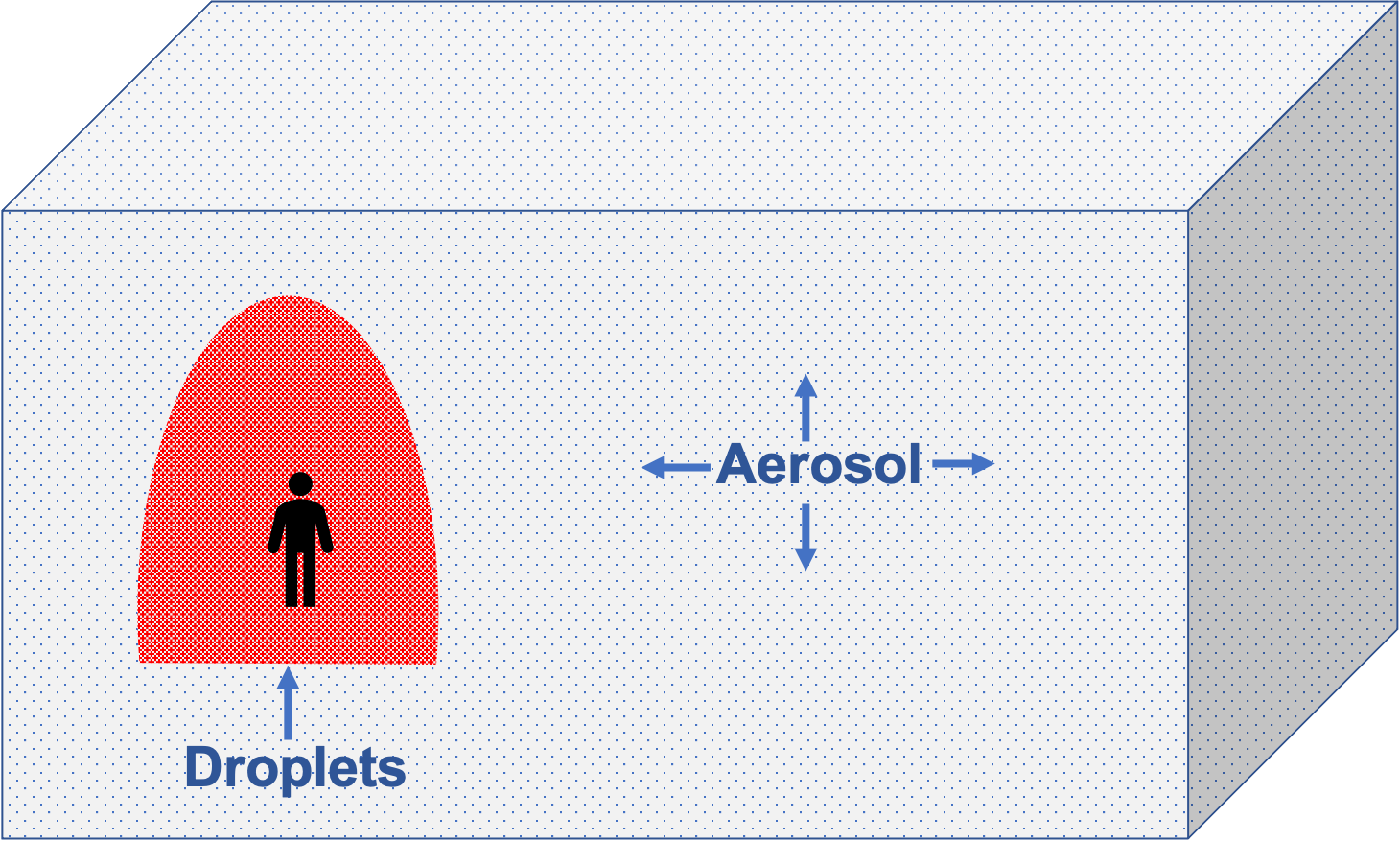
Droplets (red) spread close to an infective person while aerosols (blue) spread far.
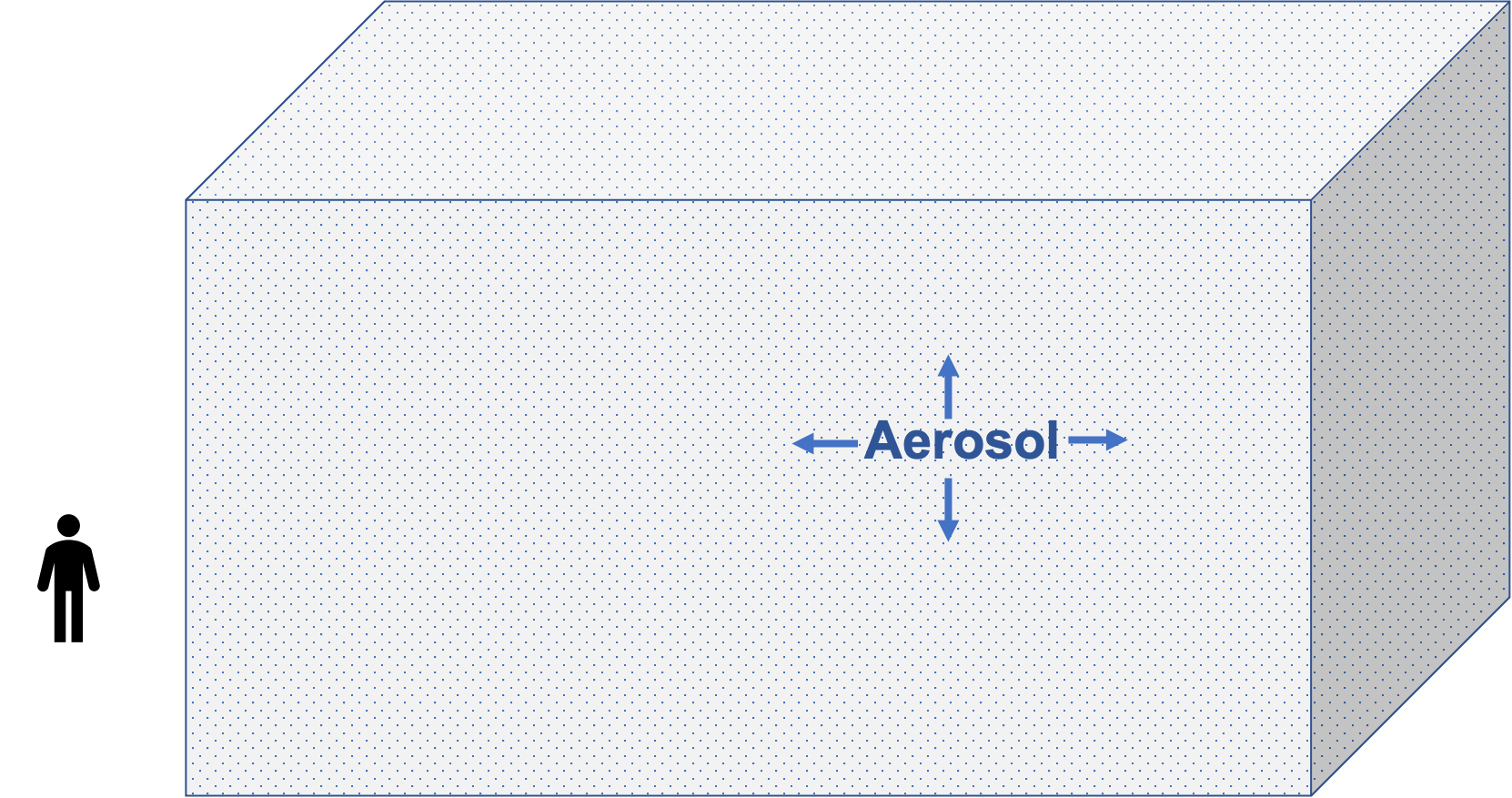
Aerosols remain in the room long after an infective person has left.
How can you minimize COVID risk?
It is quite easy to avoid COVID for most people. We provide below the most critical steps that you can take, roughly in decreasing order of priority, to help you decide on a level of risk that you are comfortable with. These suggestions are not meant for frontline workers, such as health care providers or those caring for sick persons. They are at higher risk and ought to follow the guidelines of their professions or physician, respectively.
- Social distancing: Ideally, you would isolate yourself in a cave in the Himalayas. Alternately, at least avoid people outside those you are living with. This is the most effective step. If there are no people to expose you to the virus, then you cannot get infected. But please remember that aerosols can be present if people had been present earlier. It would be best if you socially distanced yourself in space and time.
- Good masks: It may be surprising you to know that the public health advice on masks is not meant to keep you safe; it is to keep others safe from you. Much of COVID spread outside the household happens through superspreading, and you may be subject to a rather large dose of viruses then. Regular masks are too flimsy to keep you safe in such high-risk situations [Srinivasan]. However, even cloth masks confer significant benefit in many cases [Bazant] and may also reduce the likelihood of infection turning serious. So, if you don’t have a good mask, then a cloth mask is considerably better than no mask.
- What mask should I wear? If you want to be safe, you ought to use a good mask, ideally an N95 mask with ties around the head, rather than ear loops [Srinivasan]. If N95s are not available, you can use a KN95 mask. If your N95 or KN95 mask leaks a little, then you can wear a surgical or regular mask over it when you visit locations with high risks, such as health care providers.
- How should I wear the mask? Adjust it so that it fits you tightly [OSHA]. If the mask does not leak much when you breathe out, it will likely not leak much when you breathe in and so ought to be effective.
- What mask should my children wear? You may not get N95s for children that fit well. You can have them wear a surgical mask and perhaps a cloth mask over the surgical mask (not the other way around) instead. CDC recommends against masks for babies below 2 years old [CDC-3], while the WHO does not recommend masks for children below 5 years old [WHO-1]. There are risks associated with masks for babies, such as choking hazards. Consequently, babies should rely even more on social distancing.
- When should I wear masks? You ought to use good masks in any situation that you are exposed to droplets or aerosol, that is, indoor locations irrespective of whether people are present and crowded locations outdoors. Well ventilated indoor areas, say moderate-sized rooms with windows open, are at lower risk of aerosol spread than those that are not well ventilated.

Socially distanced outdoors; may be safe without masks. [Photo: by MONUSCO is licensed under CC BY-SA 2.0]

Well ventilated space; may be safe without masks. [Photo: by U.S. Army ROTC is licensed under CC PDM 1.0]

Too crowded outdoors; need masks. [Photo: by CharlesFred is licensed under CC BY-NC-SA 2.0]

Others might have shed aerosol-borne viruses earlier; need masks. [Photo: by docoverachiever is licensed under CC BY 2.0]
Social distancing and N95 masks can eliminate most of the risk of COVID for the typical person. The remaining steps are additional protections. However, if you have people come to your home, then the ventilation step too is essential.
- Ventilation: Good ventilation is necessary to let aerosols dissipate. (It will not help much with droplets, though.) It is advisable to keep windows open to the outside if you cannot avoid meeting people at home, for example, when a household help or repairman is present. Purchase a portable HEPA filter and run it while anyone is present and for a couple of hours after that. The device you buy should have the capacity to handle your room size.
- What do you mean by good ventilation? A good ventilation system would remove impure air from the room and replace it with pure air, thus eliminating aerosols. A room with windows open will often accomplish this goal. Forced ventilation, for example, passing the air through a HEPA filter, can also be effective. One caution is that forced ventilation can create a draft that brings aerosols toward a person downwind, leading to infections [Kwon]. So, you ought to avoid being downwind from others.
- Face shield: There is some evidence for COVID transmission through the eyes [Zeng]. You could consider wearing a plastic face shield along with a good mask in high-risk situations [Perencevich]. There have been suggestions that using a face shield without a mask can lead to risk by trapping viruses between the face shield and the face. So, it is essential to wear a good mask along with the face shield.
- Toilet: There is some indication that COVID might have spread in from other apartments through the plumbing system due to the familiar culprit — aerosols [Kaiser]. Make sure that you use any drains in your house at least once a week. This includes toilet bowls, sinks, floor drains, etc. Pour water in the drain, flush the toilet, and open the tap in the sink. Please keep the toilet bowl cover closed. This is especially a concern with old plumbing systems. However, this step is helpful even otherwise to prevent sewage gases from entering your house.
- Disinfecting surfaces and hands: Disinfecting surfaces and washing your hands with soap can help prevent fomite transmission. It is also advisable to shower and change clothes after visiting a location where you might have been exposed to the virus.

The second passenger to your left is wearing a face shield but a mediocre (blue) mask. It is essential to wear a good mask in indoor spaces, like the first passenger on the left, although one with ties around the head would have been better than ear loops. A face shield is helpful in high risk locations, such as hospitals. [Photo: by N509FZ is licensed under CC BY-SA 4.0]
Frequently (and infrequently) asked questions
- Mechanisms of COVID-19 spread
- If I don’t see any droplets being emitted, am I safe? Droplets are over 5 microns in diameter, which is just a tenth of the width of a human hair. So, they are usually not visible. What you don’t see can hurt you!
- What safety precautions should I take if 6 feet is not far enough? It is not feasible to perform computational fluid dynamics simulations for each location where you are present to determine the safe distance. So, it is strongly advisable to wear a good mask to reduce risk even if others are more than 6 feet away indoors. Overall, the danger from droplets is much greater in close proximity than at 20 feet away, while a significant risk from aerosols arises at an even longer distance. It is difficult to estimate a safe distance for aerosols, and so you should assume aerosol risk at any indoor location where others have been present.
- I heard that the outdoors are safe. Do I need to wear a mask outdoors? Aerosols dissipate quickly outdoors. However, if others are close by, then you would still have a risk from droplets. People have got sick amidst crowds outdoors. A good mask would be effective in crowded outdoor locations.
- My room is well air-conditioned. Is this safe? Not at all! Air conditioner filters are typically not very good. In addition, they are usually not vented to the outside. So, if you are in a closed air-conditioned room, then you could have a high risk of exposure to aerosols even if no one else is present if an an infective person had been there earlier.
- Where else am I at risk of aerosols? Any connection through the air to a location in which an infective person had been present leads to risk. Aerosols are typically removed through dissipation outdoors, a good air filter, or a time lag of several hours. If any of these conditions are not met, then you are at risk. For example, there have been indications of aerosol-based COVID spread through the plumbing system [Kaiser] and air ducts [Hwang].
- Will aerosols dissipate fast in a large indoor location, such as an airport? Recent research, and intuition, suggest that aerosol risk is lower in large rooms because they have space to dissipate [Bazant]. However, this assumes that there is only one infective person there. A large area may have more people and thus more infective persons. In that case, a large room may not reduce risk.
- Protecting yourself
- I am standing alone in a hotel lobby (or some other indoor location). Am I socially distanced? No. If people had been present there a few hours ago, then it is not social distancing because you would be vulnerable to infection through aerosol. An outdoor location without people nearby would count as social distancing, though. An indoor space vented to the outside, such as with windows open, may count as social distancing if others are not present close to you. CDC’s recommendation of 6 feet distance is not adequate indoors.
- Why do public health agencies ask us to distance ourselves from others, but not those in our own household? The virus does not care whether family, friend, or foe shed it. In fact, household transmission is the most common method of transmission. However, it is difficult to distance yourself from others in the household for an extended time. So, unless they are sick or exposed to COVID, you are not asked to take extra precautions. It is not because it is safe, but because it is infeasible.
- Can I reuse N95 masks? The filtration material of these masks lasts a long time. However, these masks may accumulate viruses if you reuse them often. So, please wash your hands after handling them, especially if you tend to put your hand in your mouth or eyes. When there was a shortage of N95 masks, CDC permitted specific procedures to disinfect these masks. Those procedures were meant for trained professionals and are best avoided at home.
- How do I figure out which mask brand to get? Any genuine N95, KN95, or FFP2 masks has filtration material that is of excellent quality. The problem arises from leaks between the face and the mask. KN95 masks limit total leak to 8%. N95 mask standards don’t limit the leakage. But N95 masks available from before the pandemic usually had minimal leakage and were much better than KN95 masks. Masks produced by new manufacturers may, perhaps, not be as good. You can find information on reliable brands for different types of masks at [FDA-1] and [CDC-4].
- Is it safe to exercise while wearing a mask? WHO recommends against it [WHO-2] for multiple medical reasons, primarily the difficulty of breathing. They also suggest maintaining a one-meter distance from others while exercising. Note that a one-meter distance is not adequate in closed indoor spaces due to aerosols, as mentioned above. Given that masks are not recommended for exercise, it is perhaps best not to exercise in closed indoor locations where others might have been present.
- Do I need to take all these precautions if I have had two doses of a COVID vaccine? We suggest that you do take these precautions even if you have had both doses of a vaccine. CDC has relaxed the mask guidance in many situations, but data from some countries indicate that vaccines don’t give adequate protection against some of the new virus variants. For example, Seychelles and Chile experienced COVID surges with around 60% and 40% of the population fully vaccinated. Vaccination does decrease the fraction of severe cases and so is certainly recommended. However, as we mentioned earlier, there are good reasons to avoid even milder cases, and one should not rely solely on vaccines for protection.
- Getting back to a normal life
- I can’t live without household help. What should I do? If you absolutely require household help, can you have that person come less frequently? A messy house may be preferable to a hospital stay! Please wear a mask while the helper is present, have the helper too wear a good mask, and use the ventilation guidelines above.
- I am a household helper who needs a job to survive. What should I do? Please use a good mask and persuade your employer to follow the ventilation guidelines above.
- I drive a taxi or bus. What should I do? Please use a good mask to stay safe from droplets and aerosols. If possible, keep the windows open. If the customer insists on air conditioning, then please open the windows after the customer leaves. You would need to keep your mask on until the polluted air is vented out.
- I will be staying in a centrally air-conditioned hotel room. Is this safe? It is very unlikely to be safe due to aerosols. There is evidence for COVID spread through air ducts [Hwang]. It is also difficult to wear a good mask for a long duration. A portable HEPA filter could help, but it is best to avoid such hotel stays.
- I will be eating at a restaurant. Is this safe? An air-conditioned restaurant is unsafe due to aerosols. There have been superspreading events with just 5 minutes of exposure [Kwon]. You can’t wear a mask while eating, and even short exposures without a mask lead to risk in superspreading situations [Srinivasan]. If you must go to a restaurant, a socially distanced restaurant with outdoor seating is best.
- Is it safe to visit a doctor or hospital for non-COVID treatment? If you take the precautions mentioned here, it is most likely safer to seek treatment than to postpone it for any issue that could have long-term impact. In addition, many doctors are making house calls. Please remember to take all precautions for visitors to your house if a health care provider visits you. You may have concerns about the availability of beds in hospitals. But hospitals usually have some beds reserved for non-COVID patients. In summary, it is not advisable to postpone essential medical care.
- Should I resign myself to a boring life? Not at all. (a) An N95 mask can keep you safe to a large extent. For example, you could go to a movie wearing this mask. (b) You can change venues where you have fun. For instance, you could exercise at the beach instead of in a gym. (c) You could decrease the frequency of activities at high risk locations. (d) You could perhaps consider expanding the set of activities that you enjoy to include those that involve solitude, such as nature hikes.
- Will I be safe if I follow all the above suggestions? The insights above are meant to help you minimize risk. However, they don’t eliminate risk. For example, an N95 mask with a tight fit could eliminate 99% of the viruses. But if you are in a location with a high virus concentration, then even this may be inadequate.
- Can you provide clarification on an issue that you have not covered here? We welcome additional feedback and questions related to non-pharmaceutical interventions.
- Other resources
- Estimate COVID risk in rooms. An app can help estimate the risk in rooms, accounting for aerosols based on the model in [Bazant]. This app does not take superspreading into account, and so your actual risk may be substantially higher.
- COVID-19 myths and facts. WHO has a reasonably good web page presenting facts related to COVID-19 [WHO-2]. But because of their neglect of aerosols, they miss out on some critical preventive measures covered on our page. Also, while interpreting their advice, please note that the absence of evidence is not the same as evidence of its absence.
- Caring for a sick person. CDC has a webapage on Caring for Someone Sick at Home.
Why are we providing this advice?
We are motivated by the second wave in India. We see much misinformation on social media. In addition, public health advisories come out much later than scientific results do. We hope that timely and accurate information will help you make decisions that are right for you.
- How are you different from thousands of other sites offering COVID advice?
- Why does your advice sometimes differ from that of public health agencies?
- In February 2020, we identified the risk of COVID importation to the USA when federal public health experts downplayed the threat.
- We recommended masks when CDC recommended against it for the general public.
- We provided evidence that the CDC’s 6-feet social distance guideline was inadequate, and that their stance against aerosol-based spread was incorrect several months before CDC acknowledged it.
- NSF RAPID grant on Leveraging New Data Sources to Analyze the Risk of COVID-19 in Crowded Locations.
- NSF CSSI grant on Cyberinfrastructure for Pedestrian Dynamics-Based Analysis of Infection Propagation Through Air Travel.
- Supercomputing time on NERSC Cori, Argonne Theta, and TACC Frontera.
- [Laxminarayan] Laxminarayan R, Wahl B, Dudala SR, et al. 2020. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science. 370 (6517):691-697. doi:10.1126/science.abd7672
- [CDC-1] Centers for Disease Control and Prevention. 8 Apr 2021. Post-COVID Conditions.
- [Zhang] Zhang L, Richards A, Barrasa MI, Hughes SH, Young RA, Jaenisch R. 2021. Reverse-transcribed SARS-CoV-2 RNA can integrate into the genome of cultured human cells and can be expressed in patient-derived tissues. Proceedings of the National Academy of Sciences. 118 (21) e2105968118. DOI: 10.1073/pnas.2105968118
- [Dbouk] Dbouk T and Drikakis D. 2020. On coughing and airborne droplet transmission to humans. Physics of Fluids 32, 053310. https://doi.org/10.1063/5.0011960
- [Bazant] Martin Z. Bazant, John W. M. Bush. 2021. A guideline to limit indoor airborne transmission of COVID-19. Proceedings of the National Academy of Sciences Apr 2021, 118 (17) e2018995118; DOI: 10.1073/pnas.2018995118
- [Kwon] Kwon KS, Park JI, Park YJ, Jung DM, Ryu KW, Lee JH. 2021. Evidence of Long-Distance Droplet Transmission of SARS-CoV-2 by Direct Air Flow in a Restaurant in Korea. J Korean Med Sci. 2020;35(46):e415. Published 2020 Nov 30. doi:10.3346/jkms.2020.35.e415.
- [Kaiser] Kaiser J. Can you catch COVID-19 from your neighbor’s toilet? Science, 4 Sep 2020.
- [Hwang] Hwang SE, Chang JH, Oh B, Heo J. 2021. Possible aerosol transmission of COVID-19 associated with an outbreak in an apartment in Seoul, South Korea, 2020. Int J Infect Dis. 2021 Mar;104:73-76. doi: 10.1016/j.ijid.2020.12.035. Epub 2020 Dec 17. PMID: 33346125; PMCID: PMC7834623.
- [CDC-2] Centers for Disease Control and Prevention. 7 May 2021. Scientific Brief: SARS-CoV-2 Transmission.
- [Srinivasan] Srinivasan A, Mubayi A and Akman O. 2020. Should N95 Respirators be Recommended for the General Public. Letters in Biomathematics. 7 (1) 143–152.
- [CDC-3] Centers for Disease Control and Prevention. 17 Sep 2020. Help Stop the Spread of COVID-19 in Children.
- [WHO-1] World Health Organization. 21 Aug 2020. Coronavirus disease (COVID-19): Children and masks.
- [OSHA] Occupational Safety and Health Administration. Last accessed 6 May 2021. Seven Steps to Correctly Wear a Respirator at Work.
- [Zeng] Zeng W, Wang X, Li J, et al. 2020. Association of Daily Wear of Eyeglasses With Susceptibility to Coronavirus Disease 2019 Infection. JAMA Ophthalmol. 138 (11):1196–1199. doi:10.1001/jamaophthalmol.2020.3906
- [Perencevich] Perencevich EN, Diekema DJ, Edmond MB. 2020. Moving Personal Protective Equipment Into the Community: Face Shields and Containment of COVID-19. JAMA. 2020;323(22):2252–2253. doi:10.1001/jama.2020.7477
- [WHO-2] World Health Organization. Accessed 16 May 2021. Coronavirus disease (COVID-19) advice for the public: Mythbusters.
- [CDC-4] Centers for Disease Control and Prevention. 4 May 2021. NPPTL Respirator Assessments to Support the COVID-19 Response.
- [FDA-1] U.S. Food and Drug Administration. Accessed 16 May 2021. Personal Protective Equipment EUAs.
- [WIRED] Molteni M. 13 May 2021. The 60-Year-Old Scientific Screwup That Helped Covid Kill. Wired magazine.
- [Chen] Chen W, Zhang N, Wei J, Yen H-L, Li Y. 2020. Short-range airborne route dominates exposure of respiratory infection during close contact. Building and Environment, Volume 176, 106859,
ISSN 0360-1323. https://doi.org/10.1016/j.buildenv.2020.106859.
For several years, we have been performing research on science-based policies to reduce viral infection risk in crowded locations such that there is minimal disruption to human activities. Consequently, we can provide insight to enable you to balance your desired activities against health risks. Note that the application of science to practical policies differs from science purely for knowledge. Published scientific papers advance scientific knowledge. They don’t represent a scientific consensus, which takes time to develop. For decision-making, one needs to take action in the presence of uncertainty and partial knowledge. Our research has focussed on this aspect. Our research has been cited in testimony to the United States House of Representatives and covered by over 300 news outlets around the world. We also engage with decision-makers regularly.
There are a variety of reasons for this, which we address below. But we first wish to point out that we have been ahead of the public health agencies on several aspects of the pandemic, such as the following.
One reason for this is that the goal of public health agencies is not to keep you healthy; it is to keep the public healthy. It is possible to have a raging epidemic in which you remain healthy and for the epidemic the die down while you get sick. Public health agencies focus on strategies that will lead to the epidemic dying down if most people follow them. Our research too follows this line generally. However, we also analyze actions that an individual can follow, which would help him even if others were to act carelessly.
Another reason for this is that many preventive steps for COVID spread are based on engineering research, which public health researchers are unacquainted with [WIRED]. Even the methodologies differ. Note that once you get exposed to the virus, it becomes a medical problem, in which techniques from health sciences are appropriate. However, the question of whether you will get exposed to the virus has a strong physical sciences component. For example, engineering researchers used computational fluid dynamics techniques to show that CDC’s 6-feet social distancing guidance was inadequate. Public health researchers are unacquainted with such methods and may not even be aware of journals where such results are published.
Finally, it takes time for scientific results to be formulated into policies. On the other hand, not all science results follow solid methodology; so, one needs to evaluate the results of a paper carefully. When we use results from others’ work, we examine their methods to determine whether they are adequate.
Acknowledgments
We acknowledge the following financial and computational resource support.
Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation or other funding sources.
